Sleeve Gastrectomy
The Laparoscopic Sleeve Gastrectomy is the most commonly performed operation for weight loss in the United States and the World. It is performed minimally invasively through very small incisions, it is an extremely safe operation, in fact it is safer than having your gallbladder removed, (which is a very common operation called a laparoscopic cholecystectomy).
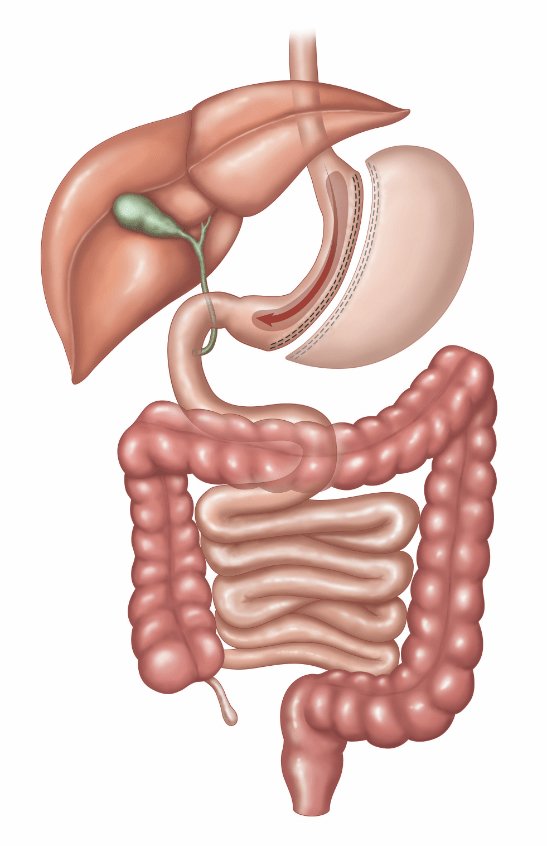
In a sleeve gastrectomy or LSG we remove approximately 80% of the stomach (an area called the greater curvature), which results in the stomach taking the shape of a tube or "sleeve" which holds much less food. More importantly, the portion of the stomach we remove is where most of the hunger hormone ("Ghrelin”) is made, as a result your Ghrelin or hunger hormone levels drop enormously after surgery. If you ask any patient who has had a sleeve gastrectomy, they will most likely tell you they “just don’t feel hungry anymore”. This “resetting” of your hunger hormones is one of the important mechanisms behind the spectacular weight loss we see after a sleeve. You can expect to lose between 60 - 70% of your excess weight (EW).
-
Most patient go home the next day, or sometimes, in selected cases some patients may go home the same day of surgery.
-
The Sleeve Gastrectomy works in a few different ways. On the one hand, the large reduction in the size of the stomach will make you feel more full quicker, but the most important mechanism of action is changing your hormones. Specifically, the hunger hormone, Ghrelin, is mostly made in the portion of the stomach that is removed.
-
The risk of mortality in a sleeve gastrectomy today is 1 in 1000, or 0.1%. Compared to laparoscopic cholecystectomy which is one of the most common operations performed in the US, which has a mortality of up to 7 in 1000 (0.7%), thus a sleeve is even safer than a very safe, very common procedure performed every day in the US!
In terms of results, most patients lose between 60-70% of their Excess Weight (EW), and the vast majority have resolution of their obesity related comorbidities, such as Diabetes, Hypertension, Sleep Apnea, High Cholesterol, etc.
Bariatric Surgery also decreases risk of many cancers including breast, colon, prostate, etc. Overall, Bariatric Surgery increases life expectancy!
-
Yes, you should take a Bariatric Multivitamin daily for the rest of your life. After Surgery, we will follow you closely at regular intervals up to the 1 year mark, and then you should have an annual follow-up visit to check vitamin levels and other routine lab work.
-
All surgeries or procedures have some risk of complications. With a sleeve gastrectomy, they occur in less than 1% of operations. Surgical complications may include:
Bleeding.
Infection.
Leaking from the staple line.
After recovering, some people may develop long-term complications from the surgery. These are usually easy to treat when they occur. They may include:
Scar tissue after the operation may cause your stomach to be too narrow, which can slow or block food from moving through your stomach causing nausea, vomiting, and difficulty eating.
Nutritional deficiencies. It’s harder to get enough nutrients when you’re eating much less. Our bariatric patients are prescribed daily nutritional supplements (a bariatric multivitamin or MVI for life.
Gastroesophageal reflux/HERD/Heartburn. Some people who had acid reflux before the operation may feel that it gets worse afterward, and some people who didn’t have it before seem to get it. Most of the time this can treated with medication called PPI (Proton Pump Inhibitor).
Gallstones. Rapid weight loss may make gallstones more likely. It causes more fat to process through your liver, which can then build up in your gallbladder as cholesterol stones which can cause pain after eating. You may need another surgery to remove your gallbladder called a cholecystectomy. This can usually be performed as an outpatient.